Purpose of treatment :
1.Improve quality of life
2.Improve outcome of life
β-blocker drug (Antiadrenegic drug)
block the action of endogenous catecholamines (epinephrine (adrenaline) and norepinephrine (noradrenaline) in particular),
on β-adrenergic receptors, part of the sympathetic nervous system which mediates the fight or flight response.
Action of β adregenic receptor (part of sympathethic nerves system)
-three known types of beta receptor, designated β1, β2 and β3.
a) β1-Adrenergic receptors are located mainly in the heart and in the kidneys.
b) β2-Adrenergic receptors are located mainly in the lungs, gastrointestinal tract, liver, uterus, vascular smooth muscle, and skeletal muscle.
c) β3-receptors are located in fat cells
Respiratory system(β2 agonists receptor)
1.bronchodilation
2. Increase Respiratory Secretions
Cardiovascular system
Heart(β1 agonists receptor)
1.Increase heart rate
2.Increase AV conduction
3.Increase BP -rise in systolic and diastolic-NA
-rise in systolic and fall diastolic-Iso
Blood vessel(β2 agonists receptor)
1.Vasodilation
1.Increase secretory activity of ciliary epithelia(caution to patient with glaucoma)
2.Increase Intraocular Pressure
GIT(not clinical significant)
1.Reduced peristalsis
2.Sphincter constricted
Bladder
1.Relaxed detrussor muscle
Uterus
1.Decrease contraction of uterus
Metabolic
1.Increase glycogenolysis- hyperglycaemia,hypelactidemia(β2)
2.Decrease insulin
3.Increase lipolysis
4.Increase lipid profile in plasma
5.Transient hyperkalemia followed by hypokalemia
CNS
Not produce any effect on CNS because poorly penetration in brain (hydrophilic)
Lipophilic drugs
Lipophilic drugs (metoprolol, propranolol, timolol) are
rapidly and completely absorbed from the gastr
ointestinal
tract but are extensively metabolised in the gut wall
and in the liver (first pass effect), so that the
ir oral
bioavailability is low (10–30%). These drugs may accumulate
in patients with reduced hepatic blood flow (i.
e.,
elderly, congestive heart failure, liver cirrhosis). Lipophilic
drugs present short elimination half-lives (1-5 h)
and they easily enter the central nervous sys
tem (CNS),
which may account for a greater incidence of
central
side-effects.
Hydrophilic drugs
Hydrophilic drugs (atenolol, esmolol) are absorbed incompletely
from the gastrointestinal tract and are excreted
unchanged or as active metabolites by the kidney.
They have longer half-lives (6–24 h), and do not interact
with other liver-metabolised drugs. They barely cross the
blood–brain barrier. Elimination half-life is increased
when glomerular filtration rate is reduced (i.e., elderly,
renal insufficiency).

Mechanism of action in IHD
The prevention of the cardiotoxic
(a) Antihypertensive action.
Associated with a decrease in cardiac
output, inhibition of the release of renin and production
of angiotensin II, blockade of presynaptic a-adrenoceptors
that increase the release of norepinephrine from
sympathetic nerve terminals and decrease of central
vasomotor activity.1–9
(b) Anti-ischaemic action
b-blockers decrease myocardial oxygen demand by reducing
heart rate, cardiac contractility, and systolic
blood pressure.10 In addition, prolongation of diastole
caused by a reduction in heart rate may increase myocardial
(c) Reduction of renin release and
angiotensin II and aldosterone production by blocking of
b1-adrenoceptors on renal juxtaglomerular cells.
(d)Improvement of left ventricular structure and function,
decreasing ventricular size and increasing ejection fraction.
6–8 b-blockers may improve cardiac function because
they:
(i) reduce heart rate, prolong diastolic filling
and coronary diastolic perfusion time,
(ii) decrease myocardial
oxygen demands,
(iii) improve myocardial energetics
by inhibiting catecholamine-induced release
of free fatty acids from adipose tissue,
(iv) upregulate
b-adrenergic receptors
(v) reduce myocardial
oxidative stress.1;11;12
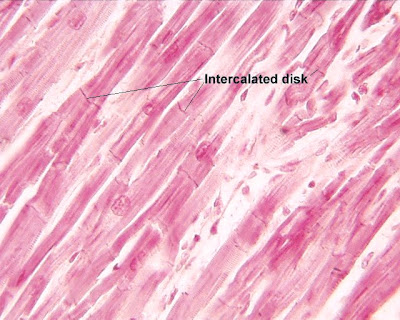
(e) The antiarrhythmic effect, the
result of direct cardiac electrophysiological effects
(reduced heart rate, decreased spontaneous firing of
ectopic pacemakers, slowed conduction and increased
refractory period of AV node),
reduces the sympathetic
drive and myocardial ischaemia, improves baroreflex
function and prevents catecholamine-induced hypokalemia.
Other mechanisms include:
Inhibition of cardiac apoptosis mediated via the activation of the b-adrenergic
pathway,
Inhibition of platelet aggregation,
Reduction of the mechanical stress imposed on t
he plaque,
Preventing plaque rupture
Resensitization of the b-adrenergic pathway and changes in myocardial gene expression,
i.e., an increase in sarcoplasmic reticulum calcium ATPase, mRNA and a-myosin heavy chain mRNA and a decrease in b-myosin heavy chain mRNA levels.15
exhibit antioxidant properties and inhibit vascular smooth
muscle cell proliferation.
Other Indication
· Angina
· Glaucoma
· Symptomatic control (tachycardia, tremor) in anxiety and hyperthyroidism
· Phaeochromocytoma, in conjunction with α-blocker
also been used in the following conditions
· Hypertrophic obstructive cardiomyopathy
· Acute dissecting aortic aneurysm
· Marfan syndrome (chronic treatment with propranolol slows progression of aortic dilation and its complications)
· Prevention of variceal bleeding in portal hypertension
· Possible mitigation of hyperhidrosis
· Social anxiety disorder and other anxiety disorders
Adverse effect
Cardiovascular
1.Reduce heart rate,
2.Extreme bradycardia and AV block.
3.Impaired sinusnode function and AV-node conduction
4.Produce cold extremities and Raynaud’s phenomenon and worsen the symptoms in patients with severe peripheral vascular disease.
5.Coronospasm
Metabolic
Hypoglycaemia -In patients with insulin-dependent type I diabetes nonselective
b-blockers mask and selective b-blocker should therefore be preferred at
least in insulin dependent patients
In one study carvedilol decreased the new onset diabetes in
patients with heart failure.
Pulmonary
Increase in airway resistance and are contraindicated in patients with
asthma or bronchospastic chronic obstructive pulmonary
disease.
Central effects
Central effects (fatigue, headache, sleep disturbances,
insomnia and vivid dreams, depression) are less common
with hydrophilic drugs
In some patients the fatigue may
be related to a decrease in blood flow to skeletal muscles;
in other cases, it may be secondary to a central effect.
Sexual dysfunction
Impotence and loss of libido.
Abrupt discontinuation of b-blockers after chronic
treatment can lead to rebound symptoms (i.e., hypertension,
arrhythmias, exacerbated angina)
This increased
Contraindications
- Asthma,
- Symptomatic hypotension
- Bradycardia
- Severe decompensated heart failure
- Chronic obstructive lung disease without bronchospastic activity
- Peripheral vascular disease are not considered as absolute contraindications and high risk patients may obtain a significant benefit from this therapy.
- Patients with heart failure and bradycardia due to sick sinus node or second or third degree AV-block may benefit from pre-treatment with pacemaker in order to tolerate b-blockers, although this approach has, however, not been formally tested.
- Diabetes or intermittent lower limb claudication are not absolute contraindications for b-blockers use
I. Non-selective β1, β2 adrenergic antagonists
Nadolol 0 Low 40–320 mg once daily
Penbutolol + Moderate 20–80 mg once/twice daily
Pindolol ++ High 10–40 mg twice daily
Propranolol 0 High + 40–180 mg twice daily
Sotalol 0 Low +
Timolol 0 High 5–40 mg twice daily
Atenolol 0 Low + 25–100 mg once daily
Betaxolol 0 Moderate 5–20 mg once daily
Bisoprolol 0 Moderate 2.5–10 mg once daily
Celiprolol + Moderate 200–600 mg once daily
Esmolol 0 Low Only i.v.
Metoprolol 0 High 50–100 mg once/twice daily
Nevibolol 0 2.5–5 mg once daily
III. α1- and β1-adrenergic antagonists
Bucindolol + Moderate 25–100 mg twice daily
Carvedilol_ 0 Moderate 3.125–50 mg twice daily
Labetalol + Low 200–800 mg twice daily
ISA: Intrinsic Sympathomimetic Activity;
i.v.: Intravenous administration possible; AMI: Acute Myocardial Infarction; CHF: Chronic Heart Failure.
Acute Myocardial Infarction (AMI)
Intravenous dosing of b-blockers
Atenolol 5 ю 5 mg Oral, 50–100 mg/day
Esmolol 0.5 mg/kg over 1–5 min 0.05–0.3 mg/kg/min
Labetalol 20 mg in 2 min 2–10 mg/min
Metoprolol 2.5–5 mg i.v. bolus over 2 min; up to three doses Oral, 25–100 mg/12 h
Propranolol 0.15 mg/kg 0.10–0.20 mg/kg/min oral, 80–240 mg/day
Practical guidance on using b-adrenergic blockers in heart failure
Who should receive b-blocker therapy
_ All patients with chronic, stable heart failure
_ Without contraindications (symptomatic hypotension or bradicardia, asthma)
What to promise
Treatment is primarily prophylactic against death and new hospitalisations for cardiovascular reasons. Some patients will
experience improvement of symptoms.
When to start
_ No physical evidence of fluid retention (use diuretics accordingly)
_ Start ACE-I first if not contraindicated
_ In stable patients, in the hospital or in outpatient clinics
_ NYHA class IV/severe CHF patients should be referred for specialist advice
_ Review treatment. Avoid verapamil, diltiazem, antiarrhythmics, non-steroidal anti-inflamatory drugs
Beta-blocker
_ Bisoprolol, carvedilol or metoprolol
Dose
_ Start with a low dose
_ Increase dose slowly. Double dose at not less than 2 weekly intervals
_ Aim for target dose (see above) or, if not tolerated, the highest tolerated dose
Starting dose mg Target dose mg
Bisoprolol 1.25 once daily 10 once daily
Carvedilol 3.125 twice daily 25–50 twice daily
Metoprolol CR/XL 12.5–25 once daily 200 once daily
Monitoring
_ Monitor for evidence of heart failure symptoms, fluid retention, hypotension and bradycardia
_ Instruct patients to weigh themselves daily and to increase their diuretic dose if weight increases
Problem solving
_ Reduce/discontinue b-blocker only if other actions were ineffective to control symptoms/secondary effects
_ Always consider the reintroduction and/or uptitration of the b-blocker when the patient becomes stable
_ Seek specialist advice if in doubt.
Symptomatic hypotension (dizziness, light headedness and/or confusion)
_ Reconsider need for nitrates, calcium channel blockers and other vasodilators
_ If no signs/symptoms of congestion consider reducing diuretic dose
Worsening symptoms/signs (increasing dyspnoea, fatigue, oedema, weight gain)
_ Double dose of diuretic or/and ACE-I.
_ Temporarily reduce the dose of b-blockers if increasing diuretic dose does not work
_ Review patient in 1–2 weeks; if not improved seek specialist advice
_ If serious deterioration halve dose of b-blocker
_ Stop b-blocker (rarely necessary; seek specialist advice)
Bradycardia
_ ECG to exclude heart block
_ Consider pacemaker support if severe bradycardia or AV block or sick sinus node early after starting b-blockers
_ Review need, reduce or discontinue other heart rate slowing drugs, e.g., digoxin, amiodarone, diltiazem
_ Reduce dose of b-blocker. Discontinuation rarely necessary
Severe decompensated heart failure, pulmonary oedema, shock
_ Admit patient to hospital
_ Discontinue b-blocker if inotropic support is needed or symptomatic hypotension/bradycardia is observed
_ If inotropic support is needed, levosimendan may be preferred
Reference
1. Cycle clinical farmacology 6th year RSMU
2.Essential of Medical Pharmacology,KD Tripathi,JAYPEE
3.wikipedia
4.Escardio(Europian Society of Cardiology)